A genetic disorder is a condition that is caused by an abnormality in an individual's DNA. Abnormalities can be as small as a single-base mutation in just one gene, or they can involve the addition or subtraction of entire chromosomes. To learn more about the different types of genetic disorders and see some specific examples, browse through the pages below
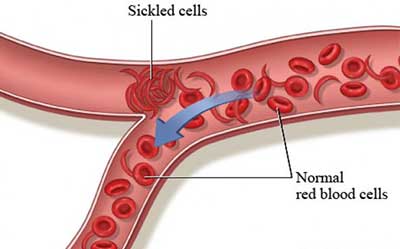
Sickle cell anemia (sickle cell disease) is a disorder of the blood caused by an inherited abnormal hemoglobin (the oxygen-carrying protein within the red blood cells). ... The irregular sickled cells can also block blood vessels causing tissue and organ damage and pain.
Sickle cell anemia is an inherited form of anemia — a condition in which there aren't enough healthy red blood cells to carry adequate oxygen throughout your body.
Unexplained episodes of severe pain, such as pain in the abdomen, chest, bones or joints.
Swelling in the hands or feet.
Abdominal swelling, especially if the area is tender to the touch.
Fever. People with sickle cell anemia have an increased risk of infection, and fever can be the first sign of an infection.
Pale skin or nail beds.
Yellow tint to the skin or whites of the eyes
Yellow tint to the skin or whites of the eyesy.
Sickle cell anemia can lead to a host of complications, including:
If you carry the sickle cell trait, seeing a genetic counselor before trying to conceive can help you understand your risk of having a child with sickle cell anemia. He or she can also explain possible treatments, preventive measures and reproductive options.


Cystic fibrosis (CF) is a genetic disorder that affects mostly the lungs, but also the pancreas, liver, kidneys, and intestine. Long-term issues include difficulty breathing and coughing up mucus as a result of frequent lung infections.
Cystic fibrosis is a progressive, genetic disease that causes persistent lung infections and limits the ability to breathe over time.
In the lungs, the mucus clogs the airways and traps germs, like bacteria, leading to infections, inflammation, respiratory failure, and other complications. For this reason, minimizing contact with germs is a top concern for people with CF.
In the pancreas, the buildup of mucus prevents the release of digestive enzymes that help the body absorb food and key nutrients, resulting in malnutrition and poor growth. In the liver, the thick mucus can block the bile duct, causing liver disease. In men, CF can affect their ability to have children.
People with CF can have a variety of symptoms, including:

People with only one copy of the defective CF gene are called carriers, but they do not have the disease. Each time two CF carriers have a child, the chances are:
The defective CF gene contains a slight abnormality called a mutation.
There are more than 1,700 known mutations of the disease. Most genetic tests only screen for the most common CF mutations. Therefore, the test results may indicate a person who is a carrier of the CF gene is not a carrier.
To couple at risk of giving birth to a child with the the disease;
Diagnosing cystic fibrosis is done through a newborn screening, a sweat test, a genetic or carrier test, and a clinical evaluation
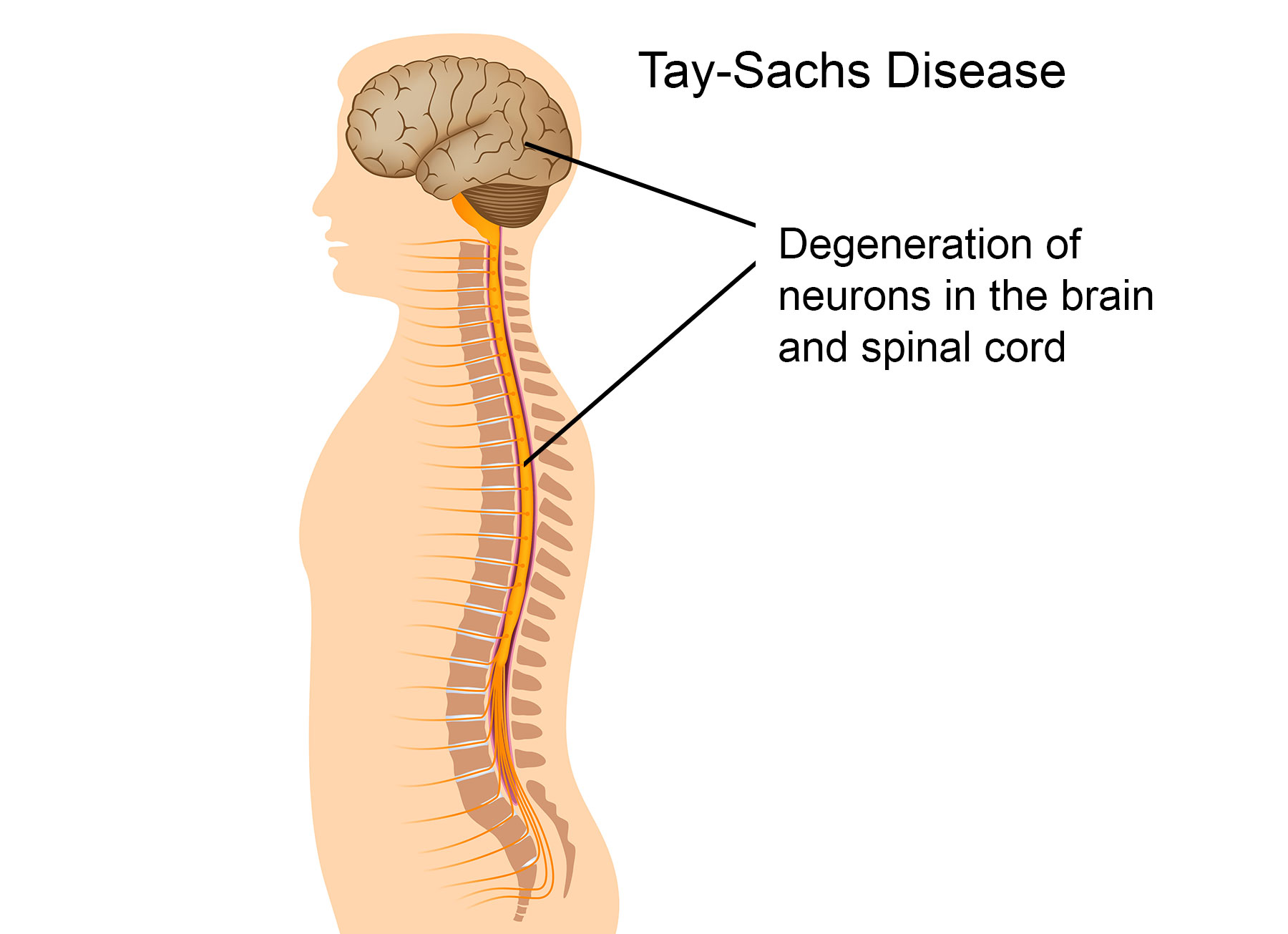
Tay-Sachs disease is a rare inherited disorder that progressively destroys nerve cells (neurons) in the brain and spinal cord. The most common form of Tay-Sachs disease becomes apparent in infancy

Healthy babies develop vision, movement, hearing, and other vital functions in part because enzymes clear out fatty protein and other unwanted material that can interfere with growth. But a baby with Tay-Sachs disease is born without one of those important enzymes, hexosaminidase A (HEXA). So, as those fatty proteins build up in the brain, they hurt the baby's sight, hearing, movement, and mental development. A child can only get Tay-Sachs by inheriting the gene for it from both parents. Tay-Sachs can be detected before birth, so couples who are thinking of having children may want to get a blood test to find out whether their child would be likely to have it.
In rare forms of the disease;
Those problems may not appear until the child is 2 to 5 years old. The disease progresses more slowly, but death usually occurs by the time the child is 15 years old.
In another, milder form of Tay-Sachs (called late-onset Tay-Sachs), the disease causes muscle weakness and slurred speech, but sight, hearing, and mental capabilities remain intact.
There is no cure for any form of Tay-Sachs disease. But doctors may be able to help a child cope with its symptoms by prescribing medicines to relieve pain, manage seizures, and control muscle spasticity.
If your child has been diagnosed with Tay-Sachs or both you and your partner are carriers of the gene, talk to your doctor or a genetic counselor about ongoing research. You also might seek support from a group such as the
National Tay-Sachs and Allied Diseases Foundation or the March of Dimes Foundation.

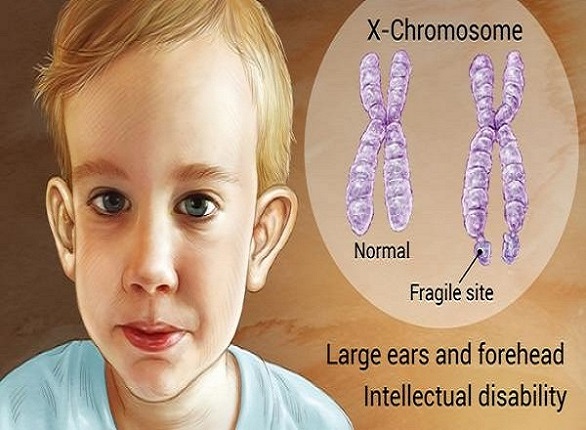
Fragile X syndrome also known as FXS, is caused by mutations in the fragile X mental retardation 1 (FMR1) gene. The FMR1 gene usually makes a protein called fragile X mental retardation protein (FMRP). FMRP is needed for normal brain development. People who have FXS do not make this protein.
FXS affects both males and females. However, females often have milder symptoms than males. The exact number of people who have FXS is unknown, but it has been estimated that about 1.4 per 10,000 males and 0.9 per 10,000 females have FXS.
Fragile X syndrome have five general categories where individuals often show altered or arrested development.
Generally people may experience:
Currently, there is no cure for Fragile X syndrome nor are there any definitive treatments other than helping the individual develop to their maximal potential through education; therapies such as speech, language, behavioral, and physical; and other therapies. Fragile X detects FMR1 DNA (PCR or Southern blot methods)
Fragile X syndrome is a genetic condition that causes a range of developmental problems including learning disabilities and cognitive impairment. Usually, males are more severely affected by this disorder than females. Affected individuals usually have delayed development of speech and language by age 2.